Table of Contents
Dr. Arthur Slutsky is a world-renowned physician-scientist whose career bridges biomedical engineering, critical care medicine, and mechanical ventilation research.
- Positions: Professor Emeritus, University of Toronto; Former VP of Research, St. Michael’s Hospital.
- Achievements: Hundreds of peer-reviewed articles, major contributions to ventilator-induced lung injury (VILI) prevention, Canadian Medical Hall of Fame inductee (2025).
- Impact: His research has shaped how clinicians worldwide manage acute respiratory failure in ICU and prehospital settings.
Quick Summary / Key Takeaways
If you remember only five things from Dr. Slutsky’s perspective, make it these:
- Airway management is foundational in critical illness — failure to secure the airway rapidly can be fatal.
- Intubation should always be approached with backup strategies: supraglottic devices and surgical airway readiness.
- Video laryngoscopy (VL) has improved first-pass success, particularly in difficult airways (Prekker et al., NEJM 2023).
- Complications are common, especially in ICU/ED settings — the NAP4 audit highlighted aspiration and failed intubation as leading causes.
- Human factors, preparation, and teamwork are as critical as technical skill for safe airway management.
SECTION 1: Fundamentals & Indications
FAQ 1: Why is airway management so critical in acute care?
Airway management is critical because without a patent airway and adequate ventilation, all other resuscitation measures are futile. The brain and heart are highly sensitive to hypoxia, and irreversible injury can occur within minutes of airway compromise. In acute care settings such as the ED or ICU, and especially in the out of hospital setting, airway interventions are often performed under less-than-ideal circumstances. Patients may be hypoxemic, hemodynamically unstable, or agitated, and clinicians may not have the preparation time typical of the operating room. Unlike controlled anesthetic inductions, out of hospital intubations frequently occur in patients with limited physiologic reserve, meaning a single desaturation episode can be catastrophic.
The importance of airway management extends beyond oxygen delivery. It also enables definitive control over ventilation, the ability to deliver inhaled anesthetics, and protection against aspiration of gastric contents. However, every airway intervention carries risk, and the margin of error is narrower in critically ill patients. Studies like NAP4 (Cook et al., Br J Anaesth 2011) highlighted that major airway complications disproportionately occur in ICU and ED settings compared with the OR.
Takeaway: Airway management is the most time-sensitive and risk-laden step in acute care resuscitation — meticulous planning and rapid execution are essential.
FAQ 2: What are the main indications for intubation in critically ill patients?
The decision to intubate should be based on three fundamental principles: (1) airway patency, (2) airway protection, and (3) adequacy of oxygenation and ventilation. Absolute indications include airway obstruction (trauma, anaphylaxis), inability to protect the airway (coma, status epilepticus, massive stroke), or respiratory failure with impending collapse. Relative indications include anticipated deterioration, where early intubation may be safer than waiting for a crash airway scenario.
In practice, common ICU indications include hypoxemic respiratory failure (ARDS, pneumonia, pulmonary edema), hypercapnic failure (COPD exacerbation, neuromuscular disease), and elective perioperative support. Non-invasive ventilation may bridge some of these cases, but thresholds for intubation should remain low when failure is likely, since delayed intubation has been associated with worse outcomes (Lee et al., Intensive Care Med 2015).
Takeaway: Indications for intubation extend beyond physiology alone — trajectory and timing are just as important in preventing adverse outcomes.
SECTION 2: Techniques & Tools
FAQ 3: How does direct laryngoscopy differ from video laryngoscopy?
Direct laryngoscopy (DL) requires alignment of the oral, pharyngeal, and laryngeal axes to obtain a direct line of sight to the vocal cords. This requires optimal positioning and operator experience; visualization can be difficult in patients with anatomic challenges (limited neck mobility, small mouth opening, obesity). Video laryngoscopy (VL), by contrast, incorporates a camera at the blade tip and projects the glottic view onto a screen. VL provides indirect visualization and generally improves the laryngeal view even when the line of sight is not ideal.
Evidence for VL has grown substantially. The MACMAN trial (Lascarrou et al., NEJM 2017) compared VL and DL in ICU patients and found no significant difference in first-pass success overall, but VL improved visualization and was particularly advantageous in difficult airways. In a more recent multicenter randomized trial (Prekker et al., NEJM 2023) VL achieved a higher first-pass success rate than DL for tracheal intubation of critically ill adults (85% vs. 71%). Rates of peri-intubation complications such as hypoxemia, hypotension, and cardiac arrest were similar between groups. The advantage of video laryngoscopy was consistent regardless of operator experience, suggesting it should be considered the preferred first-line approach in this setting.
VL also has educational benefits, as supervisors and team members can see the airway view in real time. However, VL is not fail-safe — fogging, secretions, or device unfamiliarity can still lead to failed attempts.
Takeaway: VL is increasingly first-line in critical care, but clinicians must maintain DL competence as a backup when technology fails.
FAQ 4: What is the role of supraglottic airway devices in critical care?
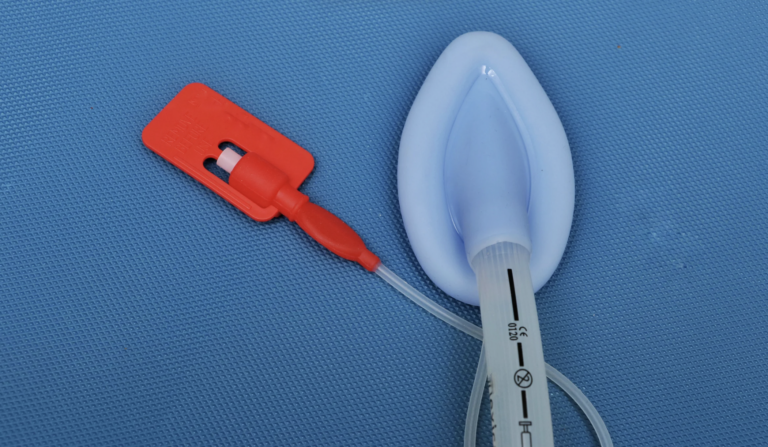
Supraglottic airway devices (SGAs) such as the laryngeal mask airway (LMA) and i-gel are designed to sit above the vocal cords, providing a secure channel for ventilation without the need for tracheal intubation. They are particularly valuable as rescue devices when intubation fails or when rapid airway control is required by providers with limited experience. SGAs can be placed quickly with minimal training and have become part of standard difficult airway algorithms. Their performance depends on the seal pressure: if airway pressures rise above the device’s leak pressure (typically 20–30 cmH₂O), gas leaks around the cuff and effective ventilation is lost. High airway pressures also increase the risk of gastric insufflation and aspiration since the seal does not fully isolate the trachea. In patients requiring higher pressures — such as severe ARDS or poor lung compliance — SGAs are usually inadequate, and an endotracheal tube is preferred.
In prehospital and cardiac arrest settings, SGAs have been studied extensively. Wang et al. (JAMA 2018) compared initial supraglottic placement with endotracheal intubation in out-of-hospital cardiac arrest and found no difference in 72-hour survival, while SGAs allowed faster placement. However, limitations include poorer airway protection against aspiration and variable efficacy in patients with abnormal anatomy or high airway pressures.
Takeaway: SGAs are indispensable rescue tools — every intubation plan should include them as part of the backup strategy.
FAQ 5: How should clinicians approach the “difficult airway”?
The ‘difficult airway’ encompasses both anatomical challenges (obesity, limited neck mobility, craniofacial abnormalities) and physiologic challenges (severe hypoxemia, hemodynamic instability, acidosis). A structured approach begins with pre-assessment tools such as the LEMON score (Look, Evaluate 3-3-2, Mallampati, Obstruction, Neck mobility). Preparation involves having all necessary equipment at hand, preoxygenating effectively, and formulating primary and backup strategies.
In the out-of-hospital setting, difficult airways must be approached with simplicity, preparation, and backup plans. Most EMS systems emphasize basic techniques first — positioning, airway adjuncts (oropharyngeal/nasopharyngeal airways), and effective bag-valve-mask ventilation. Supraglottic airway devices (SGAs) are frontline rescue tools because they are fast to place, require less training than intubation, and provide adequate ventilation in most cases. Endotracheal intubation is often reserved for highly trained providers, but multiple failed attempts increase morbidity; guidelines stress limiting attempts and moving quickly to alternatives. A “failed airway” algorithm should always be in place: after unsuccessful intubation, insert an SGA; if ventilation is still impossible, proceed to bag-mask ventilation or, in rare cases, emergency cricothyrotomy. Anticipation, early use of rescue devices, and a low threshold to stop repeated attempts are key to safe out-of-hospital airway management.
Takeaway: A difficult airway becomes manageable with anticipation, preparation, and adherence to structured algorithms.
SECTION 3: Complications & Human Factors
FAQ 6: What are the most common complications of airway management?
Airway management carries a high risk of complications, especially in critically ill patients. Hypoxemia is a relatively frequent complication and can occur within seconds in patients with poor oxygen reserves. Hypotension is also common, particularly after induction with sedatives in hemodynamically unstable patients. Other complications include esophageal intubation, aspiration of gastric contents, dental trauma, and airway injury.
The United Kingdom NAP4 audit, published in 2011 was the largest investigation of major airway complications in anesthesia, intensive care, and the emergency department. It emphasized that airway events in ICU/ED settings carried higher morbidity and mortality than those in the OR, reflecting patient fragility and the challenging environment. First-pass success is the single most important predictor of complication rates — repeated attempts greatly increase the likelihood of hypoxemia and cardiovascular collapse.
Takeaway: Achieving first-pass success and anticipating physiologic collapse are critical for minimizing complications.
FAQ 7: How do human factors and team dynamics influence airway safety?
Airway management is not just a technical skill; it is a high-stakes team activity. Clear role allocation, use of checklists, and structured communication (e.g., closed-loop commands) improve efficiency and safety. Failures often result from fixation errors, where providers persist with repeated unsuccessful attempts rather than moving to a backup strategy.
Simulation studies have shown that team training improves performance under stress. The safest airway teams are those that integrate technical expertise with effective communication, situational awareness, and humility in calling for help.
Takeaway: Human factors are as important as technical skill — teams that train together succeed together.
SECTION 4: Innovation & Future Directions
FAQ 8: What innovations are shaping the future of airway management
Airway management continues to evolve through both technological advances and systems-level innovations. Video laryngoscopy technology is improving with hyperangulated blades, disposable devices that reduce infection risk, and portable, battery-powered units for prehospital care. Fiberoptic scopes are becoming more user-friendly, and hybrid devices combining VL with suction channels are being introduced.
Beyond devices, system innovations are just as impactful. Standardized checklists, pre-intubation bundles, and real-time cognitive aids are being adopted to minimize error. Research into AI-assisted airway assessment holds promise for predicting difficulty based on facial recognition and physiologic data. Supraglottic devices are being refined with gastric drainage ports to reduce aspiration, broadening their utility.
Takeaway: The future of airway management lies at the intersection of better devices, smarter systems, and better training.
References
- Cook TM, Woodall N, Harper J, Benger J. Major complications of airway management in the UK: results of the Fourth National Audit Project (NAP4). Br J Anaesth. 2011;106(5):632–642.
- Lascarrou JB, et al. Video Laryngoscopy vs Direct Laryngoscopy in Critically Ill Adults (MACMAN): a randomized clinical trial. N Engl J Med. 2017;376:1495–1505.
- Prekker et al., Video versus Direct Laryngoscopy for Tracheal Intubation of Critically Ill Adults. N Engl J Med. 2023 Aug 3;389(5):418-429.
- Wang HE, et al. Effect of a Strategy of Initial Laryngeal Tube Insertion vs Endotracheal Intubation on 72-Hour Survival in Adults with Out-of-Hospital Cardiac Arrest: A Randomized Clinical Trial. JAMA. 2018;320(8):769–778.
- Lee J, et al. Association of timing of intubation with outcomes in patients with severe respiratory failure. Intensive Care Med. 2015;41:623–632.

Haris Shekhani MD, MBID
Haris Shekhani, MD, MBID
- Haris Shekhani MD, MBID
- Haris Shekhani MD, MBID
- Haris Shekhani MD, MBID
- Haris Shekhani MD, MBID
- Haris Shekhani MD, MBID
- Haris Shekhani MD, MBID
- Haris Shekhani MD, MBID
- Haris Shekhani MD, MBID
- Haris Shekhani MD, MBID
- Haris Shekhani MD, MBID
- Haris Shekhani MD, MBID